Insights from Washington, DC
1 | AI Graduates From Buzzword to Practical Workhorse
The FDA’s new generative-AI system, Elsa, currently has over 6,000 active internal users. It enhances the agency’s processes by supporting faster clinical protocol and submission reviews as well as label comparisons.
Other industry technology players are collaborating to leverage agentic AI to speed up clinical trials by integrating protocol design, predictive safety signal identification, patient enrollment optimization, and literature review automation. There have been remarkable achievements in AI-assisted literature reviews as regulatory prep, demonstrating 100% recall and 93% precision, reducing manual effort by up to 70%.
For those concerned that AI would replace humans, don’t worry. Be encouraged! For AI to be used effectively, accurately, and credibly, humans need to remain in the loop (“human in the loop” is the catchphrase). However, humans who know how to use AI may replace those who do not.
Note to sponsors who use AI in data mining or summarizing: the FDA has emphasized transparency and traceability, requiring clear documentation of AI algorithms and data sourcing. Bottom line: data verification becomes more important than ever. Cue the human in the loop.
When expanding processes to include AI, keep in mind that successful integration involves building organizational trust, selecting the appropriate AI tools to drive business value, and implementing rigorous frameworks for continuous monitoring and reliability assessment. Several presenters highlighted the importance of addressing challenges such as bias, hallucinations, outdated data, and regulatory uncertainties through comprehensive oversight.
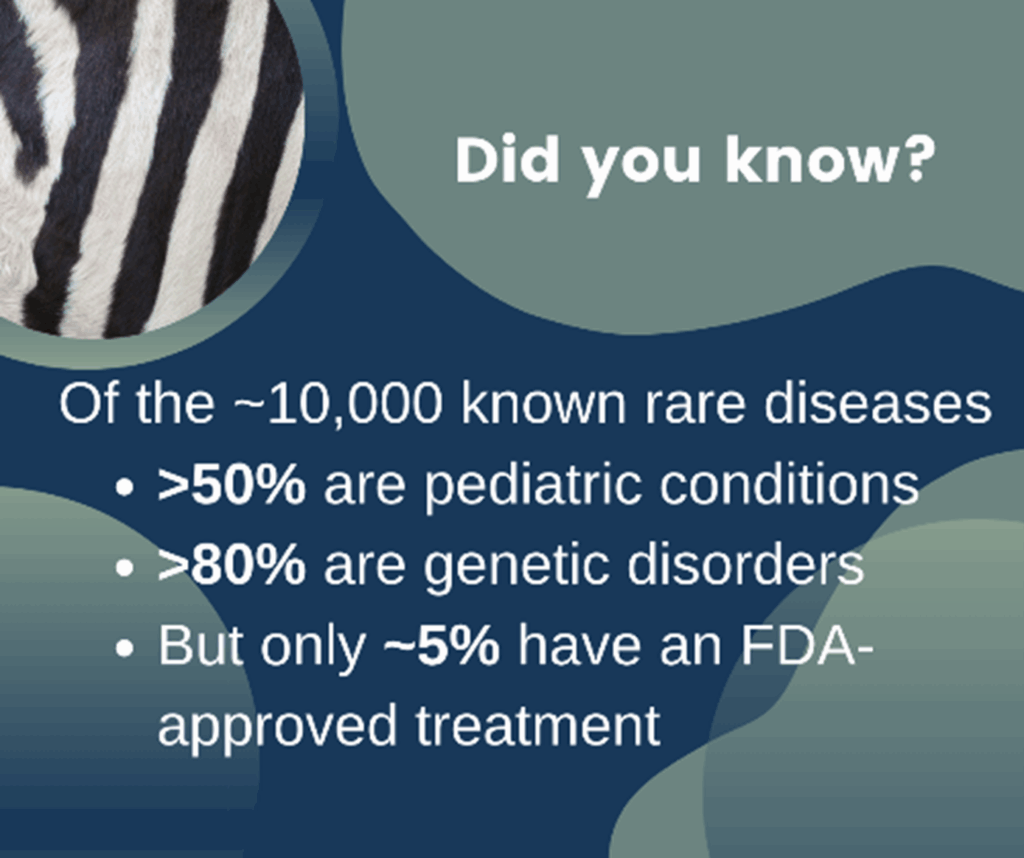
2 | Rare Diseases Accelerate With New Regulatory Pathways
Only 5% of more than 10,000 rare diseases currently have FDA-approved therapies. To encourage rare disease research and bring effective medications to patients faster, FDA Commissioner Marty Makary previewed a new “plausible mechanism pathway” to seek conditional approvals without requiring full phase 3 trials, complemented by intensive real-time patient monitoring.
Although the chatter around rare disease research was primarily optimistic, challenges persist. Notably the Inflation Reduction Act (IRA) unintentionally discourages innovation in orphan drugs, particularly affecting small-molecule investments. A major takeaway from DIA was the urgent need for modernizing newborn screening programs, which are critical for early diagnosis of rare pediatric conditions.
Adaptive trial designs, informed by disease natural history, translational science, and precise endpoint characterization, emerged as essential strategies to navigate uncertainties inherent in drug development for rare diseases.
3 | FDA Promises Agility and Collaboration
“Engage with FDA early and often” was repeated frequently throughout the conference by FDA presenters. Commissioner Makary noted a simple 15-minute phone call with FDA reviewers can save months of work. The FDA is facilitating more frequent and earlier Type-D digital interactions, enhancing efficiency in drug review processes. Incorporating early interactions can help integrate patient reported outcomes (PROs) and patient experiences into FDA submissions.
EMA is also implementing new legislation designed to simplify regulatory processes, foster innovation, and amplify patient involvement, reinforcing a global shift toward agile and proactive regulatory environments.
EMA is also implementing new legislation designed to simplify regulatory processes, foster innovation, and amplify patient involvement, reinforcing a global shift toward agile and proactive regulatory environments
4 | Patient Voices Move From Advisory to Essential
The FDA emphasized the importance of patient-focused drug development (PFDD), advocating patient experiences and preferences to shape clinical endpoints, benefit-risk assessments, and reimbursement strategies. The patient voice is increasingly influential not just in trial design but also in payer coverage and reimbursement decisions, highlighting the strategic importance of patient involvement in the process.
Patients want to be viewed as active participants rather than mere regulatory checkboxes when engaging with the industry about clinical trials. Patients can contribute their lived experience to shape a target product profile, which, in turn, will shape a strong clinical development plan. Several sponsors have patient representation on all their clinical programs. By including patient perspectives on outcomes and improving participation in clinical trials, Roche has successfully included PRO safety data in FDA submissions, with some data presented in the label.
Takeaway
The varied programs presented at DIA 2025 have highlighted transformative shifts in AI-driven processes, announced initiatives in accelerating drug development for rare diseases, proposed regulatory flexibility, and supported patient empowerment. Pharma is shifting toward rapid, iterative, and collaborative approaches, driven by high-quality data, active patient involvement, and careful technological integration.
Email us if you want to discuss the potential implications for your 2026 business!

